Mastering the Clinical Trial Feasibility Process
Clinical trial feasibility comes down to a simple question: if a sponsor runs a clinical trial at a research site, will that trial succeed?
However, answering that simple question is a complicated process. Sponsors have to determine which research sites have the participants, staff, expertise, and technology to successfully conduct their studies, and sites have to decide which clinical trials they are willing to tackle with the resources they have.
Historically, sponsors and CROs have struggled to determine site feasibility. 70% of clinical trials experience start-up delays, 80% don’t complete the enrollment phase on time, and 45% miss their projected end dates.
If research sites want to be chosen for trials, they need to understand what qualities sponsors are looking for. They also need to evaluate their resources and determine which trials are a good match for their site. Here are a few tips to help your team conquer the clinical trial feasibility process.
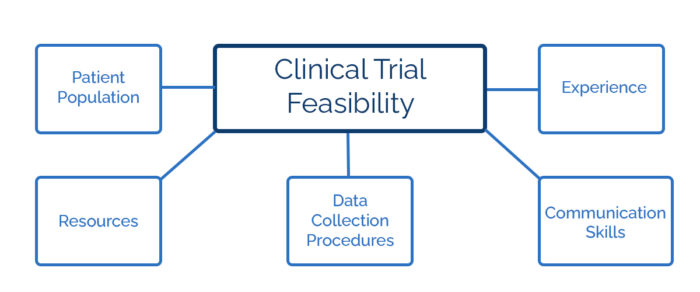
What do sponsors mean when they talk about clinical trial feasibility?
To determine clinical trial feasibility, sponsors look at sites’ patient populations, resources, data collection procedures, communication skills, and experience.
But even the best research sites can’t excel at all of these areas equally. Research sites often run dozens of clinical trials while caring for patients who aren’t enrolled in studies. This means that sites need to know which areas they should concentrate on to improve their clinical trial feasibility.
Researchers from Copenhagen University Hospital surveyed multiple sponsors and CROs to determine which traits they valued most when looking at clinical trial feasibility. 84% of sponsors and CROs responded that patient recruitment was their number one priority when choosing research sites.
Sponsors and CROs also said that a strong pool of eligible patients was more important than the research site’s level of experience. 75% of sponsors said that they would work with an inexperienced trial site if that site could offer a large patient population. 88% of sponsors also said that they would rather reach their enrollment goals 10% faster than cut their costs by 20%.
This study mainly focused on sponsors in Nordic countries, but given how often clinical trials struggle with patient recruitment, it’s safe to say finding patients is a priority around the world. Even if research sites don’t have world-famous physicians or cutting-edge equipment, they may still be selected for a clinical trial if they have a large, diverse patient population.
What do sponsors value most?
Before sponsors determine the feasibility of a clinical trial site, they must determine which features are most important for the clinical trial. If the disease being treated is rare or a trial uses precision medicine, the research site’s patient population will be most important.
For trials that involve common medical conditions, sponsors may want to focus more on what technology a research site has or how experienced their staff is. Only sponsors and CROs can determine which factors to prioritize. But to increase patient recruitment, retention, and diversity, they should be guided by the study’s needs, not just by how familiar they are with a site.
Sponsors and CROs can also save time and money by evaluating clinical trial feasibility using technology. For example, sponsors and CROs could look up a site’s information in the Shared Investigator Platform to see if a site has essential capabilities. Then they can send more detailed questionnaires exclusively to sites that meet their basic criteria.
Although in-person site visits are a possibility again, sponsors may also be able to use remote site evaluations in the early stages of the feasibility process. For example, research staff could fill out a walkthrough exercise about their departments and equipment and share their results with the sponsor through an online portal.
Doing this process online instead of in person saves sponsors time and money and ensures sites don’t have to rearrange their schedules to show a monitor around.
How can sites evaluate their clinical trial feasibility?
Guides to clinical trial feasibility often emphasize how sponsors decide if a site is feasible. While that decision is important, sites also have to decide whether they have the time and resources to take on a particular study.
For example, The Nationwide Children’s Hospital conducts an internal feasibility evaluation for every research study. They examine whether they have the correct number of staff and a strong patient pool, as well as whether the study could benefit participants. They also discuss whether there are competing studies that would draw on the same patients.
Dr. Viraj Rajadhyaksha, who has evaluated research sites for Pfizer and Astra-Zeneca, recommends that sites look closely at study designs, regulatory and ethical challenges, timelines, and community partners before committing to a study.
Many academic medical centers have developed their own clinical trial feasibility checklists. If your site doesn’t have one, you may want to work with your team to create one.
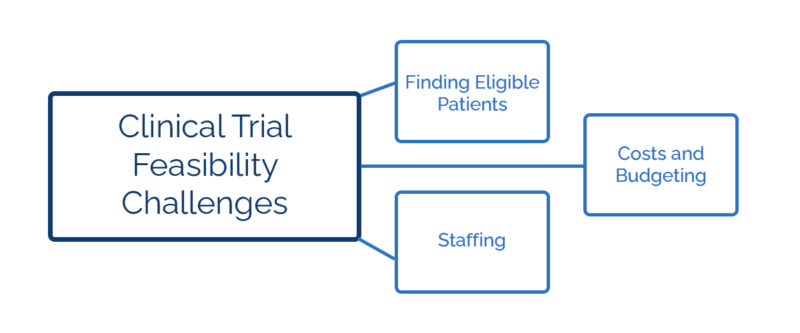
Clinical trial feasibility challenges: finding eligible patients
Finding eligible patients is critical to both sponsors and research sites, but it’s not easy. When determining feasibility, research sites often look at the number of patients at their site who have a specific disease. However, when they account for inclusion and exclusion criteria, they often discover that they have fewer patients than they realized.
Sites can also overestimate how many eligible patients will want to participate, especially if the study requires a large time commitment or involves a placebo. Sites need to send sponsors realistic estimates of their patient population that account for inclusion criteria and patients simply not wanting to participate.
If sites overestimate their eligible patient population, they will likely underestimate their recruitment timelines, leading to frustration from the sponsor and the trial being delayed.
Research sites may need to use creative recruitment methods to increase enrollment, including websites, ads, personalized letters, and reaching out to local clinics. Sites should make sure the sponsor can cover those costs before agreeing to a study.
Technology can also help with the problem of recruitment. For example, an article in Trials suggests that research sites can search electronic health records to get accurate feasibility numbers. If the EHR data is standardized, sites can set filters to automatically see how many patients are eligible for studies.
For more on how technology can help with recruitment and patient engagement, check out our guide to healthcare software here.
Clinical trial feasibility challenges: staffing
Research sites often underestimate how many hours a clinical trial will require from their staff. Principal investigators need to make sure they have enough time to meet all of a study’s protocol requirements, which may include patient check-ins, monitor visits, and signing off on logs and reports.
Giving PIs the ability to sign documents remotely will help with these challenges, but can’t eliminate them.
Sites also need to think about additional services requested by the protocol. For example, if the protocol calls for patients to have surgery and physical therapy, the site will need to look at the physical therapists’ and surgeons’ schedules before determining the clinical trial’s feasibility.
Working with monitors can also require a great deal of time from clinical research assistants or clinical research coordinators. In-person visits require CRAs or CRCs to show monitors around and guide them to where documents are stored. If sponsors opt for remote monitoring but don’t have an integrated software system, CRAs and CRCs may find themselves copying, scanning, faxing, and emailing documents.
When sites and sponsors use integrated software, can alleviate some of the challenges of remote monitoring. With the right remote monitoring technology, sites can give sponsors access to see their documents as soon as they’re updated. This way, sponsors will always have the newest versions of trial documents, and CRCs or CRAs won’t have to waste time scanning or emailing data.
Clinical trial feasibility challenges: costs and budgeting
Sponsors pay for research sites’ clinical trial expenses, but it’s important to have an accurate projection of what those costs will be. Sites constantly needing more money to complete a trial can be frustrating for both sites and sponsors.
Here are a few costs that sites and sponsors sometimes underestimate when determining feasibility:
1. Start-up costs
Start-up costs remain roughly the same whether the study enrolls many patients or just a few. All of the patient screenings, staff evaluations, and equipment inventories to determine feasibility take time. Effective healthcare software can reduce start-up costs, but not eliminate them.
2. Medical procedures
If a trial requires repeated procedures performed by nurses, physicians, specialists, or surgeons, costs will be much higher. Therefore, sites will need to double-check that the sponsor has offered enough funding to pay all of the professionals involved and to cover all procedures.
4. Adverse event reporting
Sites don’t always account for how much time adverse event reporting requires, especially serious adverse event reporting. Sites should account for these costs when determining whether the sponsor has given them a sufficient budget to make the trial feasible.
5. Costs for out-of-town participants
Lower-income patients are less likely to participate in clinical trials, possibly because they can’t afford additional costs like transportation. Clinical research sites need to confirm that sponsors will provide funding for gas or public transit, hotels, and meals when patients need them. Sponsors may also need to provide hotel accommodations for parents or children if a patient has to stay overnight.
By planning for costs that often get forgotten, sites can ensure that a clinical trial is feasible for them while sponsors decide whether the site is a good fit.
Streamlining the Clinical Trial Feasibility Process
The clinical trial feasibility process is time-consuming, expensive, and necessary. But when sponsors narrow down the attributes that are most important to them and trial sites are realistic about which studies they have the resources for, the process becomes far more efficient. Clinical trials get underway faster, and those trials have a better chance of finding and retaining the patients that they need.
To learn more about how software can help with the clinical trial feasibility process, check out our complete guide to remote site access and study start-up.