Decentralized Clinical Trials in a Post-Pandemic World: Interview with Amir Lahav
Now that COVID-19 vaccines are available, many sponsors and research sites have started to wonder which elements of remote clinical trials should stay and which ones need to be left behind. Blake Adams, VP of Marketing at Florence, sat down with Amir Lahav on The Next Phase podcast to find answers to these questions.
Amir Lahav has spent almost 15 years working in the clinical trial industry, serving at institutions from Harvard Medical School to Pfizer. Now Head of Digital R&D at Mitsubishi Tanabe Pharma Holdings America, Amir has become a passionate advocate for remote technology and flexible clinical trials. Here’s part of what he had to say (and if you want to hear it all, listen in here):
What drives your passion for decentralized trials?
I started my career as a clinical neuroscientist. I’ve always been fascinated by how the brain is shaped by our personal experiences: what we do, what childhood traumas we have, what interactions we experience in daily life.
So that drove me into neuroscience brain imaging. After my doctorate I did a postdoc at Harvard Medical School, where I learned a lot about brain imaging and how we can use different technology to study the brain.
At the time technology wasn’t “cool,” and we didn’t talk about digital health or digital therapeutics. The technology was still very interesting, though.
But what really drove me into clinical trials and the pharmaceutical industry and what I’m doing now, decentralized trials, was my first job at Pfizer. It was an amazing company to work for, with a lot of learning opportunities working with great people and leaders in the field.
And that is what led me to what I’m doing today as a consultant for companies in the digital health and digital therapeutics space. Listen to the entire conversation on our podcast here.
What does the term “decentralized trials” mean for the future of clinical research and clinical trial operations?
The concept of decentralized trials isn’t new. But I think COVID definitely was a game-changer.
A couple of years ago I tried to talk about using technology for remote patient monitoring, and a lot of site teams who were doing clinical operations weren’t sure about doing eConsent and screening and enrollment remotely.
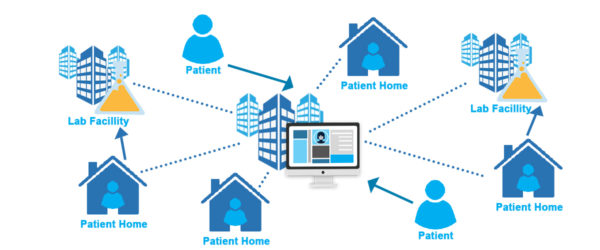
But now people realize you can enroll patients anywhere in the world, and you don’t have to bring them to the clinic. You actually collect data in the real environment where they live. You can be there 24/7 instead of taking snapshots in the clinic.
If patients come for a physical visit every 3 months or every 6 months and you get a picture of how they’re doing, that picture could be very misleading because there’s so much happening in between. With remote trials you can use wearable technology or phone data to check the health status of the patient and you can be there every day.
I would just say, why compromise on a snapshot when you can get the whole movie? Listen to the entire conversation on our podcast here.
Do decentralized trials mean not bringing patients to the site?
No, I’m not saying don’t bring patients to the clinic at all.
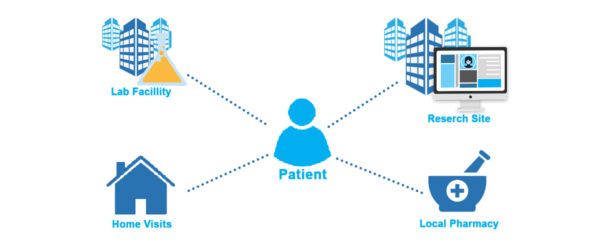
This is not a binary decision. But if you really want to know how somebody is feeling, the hospital is not necessarily the right place. It may be the right place for a blood drawing, and there’s a very low likelihood that somebody will relocate an MRI machine into your apartment building, so for that you’ll have to go to the hospital. But we can definitely minimize those visits.
That’s why COVID was a game-changer. There were people who resisted at the beginning or were skeptical, saying we’re not sure if this approach will actually stick. But COVID made it almost impossible for patients to come to the trial site, for obvious reasons, and companies needed to COVID-proof their studies. So they ended up adopting the decentralized approach whether they wanted to or not. And then they saw that there were lots of benefits to decentralized trials that they didn’t see before. Listen to the entire conversation on our podcast here.
With all the sponsors and research sites Florence works with, we see everybody approaching decentralized trials a little bit differently. How do we create some shared learnings and some operational efficiencies between companies that are approaching this decentralized space?
A lot of companies aren’t using patient notes to inform the design of the clinical trial, and patients are going to be the key for building this consortium and collaboration.
The need to compete is good for drug development overall, and confidentiality is important. We shouldn’t know about other companies’ clinical assets.
But when it comes to operations, how we do clinical trials, that should be company-agnostic and even drug-agnostic because patients are patients. It doesn’t really matter if it’s an Alzheimer’s patient or a Parkinson’s patient or a cancer patient: many patients have the same or similar needs, and they would appreciate more flexibility in the clinical trial, and they would appreciate people listening to their preferences.
And this is where pharma can do better, I think, by working together collaboratively and sharing information, especially about what didn’t work. If companies become more open, we can learn from each other and even establish some guidelines that could make clinical trials better for more patients.
Because every time you give a patient a compromised experience in a clinical trial, the likelihood that patient will want to participate again is lower. So step one is to really collaborate and share information in a more structured way, like through a website where other companies can go and find information. Listen to the entire conversation on our podcast here.
What do you think sponsors should do differently in the future?
I think pharma should learn from other industries. Pharma in general is very slow to adapt.
Companies are protocol-oriented and they have an SOP (standard operating procedure) for almost everything. They’re afraid of protocol deviation. But I would encourage everybody to build flexibility into clinical trial protocols so you won’t have to file a deviation everytime something goes a little differently.
We must treat patients in clinical trials as our customers, because if we don’t treat them very well, we won’t be attractive to them. And if we won’t be flexible, they may go with a competitor and do their clinical trial that offers more flexibility.
For example, say we have a cancer patient in the clinical trials, and as part of their schedule of activities, a nurse comes to their house and draws blood. But this patient happens to be in the area of Mass General Hospital because he’s visiting his grandson today, and he wants to go in and get the blood drawn there.
We want to allow that. We don’t want to intimidate the team and say all this is going to be a protocol deviation. And this flexibility is possible if the language of the protocol says, “test blood either at home or at the hospital.”
I think pharma should work together to change the mindset of being so strict about the operational aspects of clinical trials. Listen to the entire conversation on our podcast here.
I know you have a background in pediatric clinical trials. How do pediatric trials and decentralized trials come together to create more access and more capabilities?
I’m really glad you asked me about pediatric trials because I think they deserve much more attention. When I was a professor of pediatrics at Harvard, the first thing I learned is that children are not small adults. They require a different approach.
First, you’re not dealing with the patient alone. It’s a patient and parent dyad. The person actually signing the consent form is not the patient, and there are a lot of activities during the trial that the child has to do but the parents have to supervise.
So on platforms that help with patient monitoring, who are you going to send the reminder to? Are you going to send it to the parents? Are you going to send it to the kids who are participating in the trial?
But it all starts with the consent form, and I don’t think digitizing a consent form and turning it into a PDF is enough. I really want the kids to be able to understand what they are committed to.
A lot of the remote platforms are designed for adults, and there is room to adapt to the pediatric population so we can really put the patient at the center. For example, we can make a 60-second animated video that conveys why you’re doing what you’re doing and what the procedures of the trial are in a kid-friendly way, and send it to kids on their devices. Listen to the entire conversation on our podcast here.
In 10 years, what is the big thing that you hope to see from the clinical research industry?
I’m not sure how we’re going to perform clinical trials in 10 years, but I think that digital platforms will be more interactive and will rely much more on data that is collected from the patient’s phone.
There will be many more health apps that collect information about how the patient’s doing and the choices that patients are making on a daily basis. I also hope that patients will have the opportunity to get some of the data back. That’s something we haven’t done very well in most trials. We keep the data to ourselves, but patients deserve to see and understand their own data. Listen to the entire conversation on our podcast here.
Learn What Experts Think About the Future of Decentralized Clinical Trials
To hear Amir’s full interview, including his takes on what sponsors can learn from Amazon and how smartphones may help investigators find better treatments for Parkinson’s, check out Florence Healthcare’s Next Phase podcast. Twice a month we sit down with leaders in medical research to discuss the latest innovations in clinical trials. Subscribe on Spotify or Apple Podcasts if you don’t want to miss an episode.
For more information on how clinical research teams are preparing for the future of decentralized clinical trials, check out our decentralized clinical trials for research sites eBook.